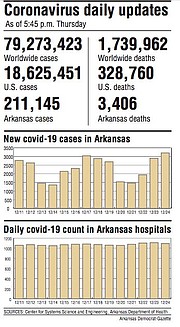
Arkansas' count of coronavirus cases rose by more than 3,200 on Thursday, breaking the record for a one-day increase that had been set just a week earlier.
The state's death toll from the virus, as tracked by the state Department of Health, rose by 30, to 3,406.
After reaching a new high on Wednesday, the number of patients hospitalized in the state with covid-19 fell by 17, to 1,093.
Those patients included 178 who were on ventilators, up from 174 a day earlier.
The state's count of cases rose by 3,204. The previous record for a one-day increase was the 3,039 cases that were added Dec. 17.
"I think the record number of cases is very distressing," state Epidemiologist Jennifer Dillaha said.
"It is not the Christmas gift I was hoping for."
[CORONAVIRUS: Click here for our complete coverage » nwaonline.com/coronavirus]
In a tweet, Gov. Asa Hutchinson said vaccines and vigilance are the "two keys to victory over the virus."
"We must be vigilant even during this special season of the year," Hutchinson said.
"Vaccines are coming, but we all must be careful to keep our loved ones safe."
The spike in cases came during the second week of the state's effort to distribute its first doses of the coronavirus vaccine, which has been initially earmarked for health care workers, as well as residents and workers in long-term care facilities.
Under the order the state submitted to the U.S. Centers for Disease Control and Prevention late Wednesday, the 23,400 doses of the Pfizer vaccine that the state will receive next week will go to hospitals, with some receiving direct shipments and others getting it through pharmacies, Dillaha said.
Health care workers in hospitals located in prisons around the state will be among those receiving the shots, she said.
She said other hospitals can administer the vaccine to high-risk workers in affiliated clinics.
Once high-risk workers at hospitals have received the shot, she said she's hopeful the state can begin making the vaccine available to workers at primary care and urgent care clinics that aren't affiliated with hospitals.
"I'm very anxious to get vaccine to the primary care clinics because they have some of the highest risk workers," Dillaha said.
VACCINE PLANS
The state's first allocation of the Pfizer vaccine, consisting of 25,350 doses, arrived in the state last week and was also designated mainly for workers at the general, acute-care hospitals.
This week's 18,525 Pfizer doses were earmarked for high-risk workers at rehabilitation hospitals, psychiatric hospitals, long-term acute-care hospitals and surgical hospitals.
Some hospitals that received doses last week received additional doses this week.
The allotment also included 1,950 doses that the Health Department will distribute to ambulance workers, including at events around the state starting Saturday.
The state this week also received its first allotment -- about 51,000 doses -- of the Moderna vaccine.
Nursing home residents and workers are first in line for those shots, followed by residents and workers at centers for people with significant intellectual disabilities and those at assisted-living facilities.
The state expects to receive an additional 17,700 doses of the Moderna vaccine next week that will also be designated for workers and residents at long-term care facilities.
Once the vaccine has been made available to high- and medium-risk health care workers and long-term-care facility residents and workers, the state will begin distributing it to the next priority groups, Dillaha has said.
Dillaha said high-risk workers include those who provide care to patients who have covid-19 or are likely to have it, people who perform procedures placing them at increased risk of infection and nonclinical staff members, such as clerks or janitors, who work around covid-19 patients.
Following the recommendation of an advisory panel, the CDC said Tuesday that the next priority group -- "Phase 1b" -- should include people 75 or older and "front-line essential workers," such as firefighters, police, prison workers and those working in manufacturing and grocery stores.
Dillaha said Wednesday that it could be "well into January" before the state moves to that phase, with the amount of time depending on how much vaccine is available and how many people who are eligible for the shot decide to take it.
LAWMAKER INFECTED
Among those who have tested positive recently is state Rep. Bruce Coleman, R-Mountainburg, House spokeswoman Cecillea Pond-Mayo said.
[Interactive Arkansas map not showing up above? Click here to see it: nwaonline.com/arvirus]
Coleman informed House Speaker Matthew Shepherd, R-El Dorado, of the test result Thursday morning, Pond-Mayo said.
She said Coleman is quarantining at home and Shepherd reported that Coleman indicated that he "is doing well." Coleman is 78.
He could not be reached immediately Thursday afternoon for comment by telephone.
During the past three months, 17 state lawmakers have acknowledged testing positive for the coronavirus.
Since the pandemic arrived in the state in March, 21 lawmakers have said they tested positive for covid-19. The Legislature includes 135 lawmakers.
ACTIVE CASES RISE
The cases added to the state's tallies Thursday included 2,358 that were confirmed through polymerase chain reaction, or PCR, tests.
The other 846 were "probable" cases, which include those identified through less-sensitive antigen tests.
The state's cumulative count of cases rose to 211,145.
That comprises 177,140 confirmed cases and 34,005 probable ones.
The number of cases that were considered active rose by 862, to 23,378, as new cases outpaced recoveries.
Pulaski County had the largest number of new cases, 338, followed by Benton County with 320, Washington County with 287, Craighead County with 139, and Faulkner County with 121.
Among prison and jail inmates, the state's count of cases rose by 116.
The state's death toll rose by seven, to 2,946, among confirmed cases and by 23, to 460, among probable cases.
The number of people who have ever been hospitalized in the state with covid-19 rose by 53, to 10,879.
The number of virus patients who have ever been on a ventilator rose by three, to 1,166.
At a record level since Wednesday, the average number of cases added to the state's tallies each day over a rolling seven-day period rose by 24, to 2,372.
VISITATION EXPANDED
As the first vaccines began being administered to the nursing home residents and workers this week, the Health Department revised its rules to allow "expanded visitation" at more long-term care facilities.
Since Oct. 6, routine visits by the family and friends of residents at nursing homes, assisted-living facilities and other long-term care facilities have been prohibited at facilities where a resident or staff member has tested positive within the past 14 days.
The revised rules, dated Wednesday, shorten that period to the past 10 days.
Rachel Bunch, executive director of the Arkansas Health Care Association, said the change brings the rules in line with the state's quarantine requirements for people who have been near someone with the virus.
Following revised guidance from the CDC, the Health Department said people without symptoms could quarantine for 10 days instead of 14 days.
That period can be shortened to just seven days if the person has a negative test for the virus from a sample collected at least five days after the exposure.
According to a Health Department report, 135 of the state's nursing homes and assisted-living facilities -- almost half the total -- had had at least one staff member or resident test positive within the past 14 days as of Monday.
"We definitely support this change and updating this guidance," Bunch said. "I think it will positively impact a lot of residents in these facilities to allow for more visitations with their families."
She said she's hoping that vaccinations of residents and staff will lead to further revisions to the rules.
Several nursing homes began administering the shots this week, after the state received its initial allocation of 51,000 doses of the Moderna vaccine.
Many more homes will hold vaccination clinics Monday, Bunch said.
"It's certainly our hope that this is the first step toward reopening and some sense of normal again," Bunch said.
Regardless of the number of cases at the facility, the new rules continue to require facilities to allow visits by family members and friends that are medically necessary "as determined by the resident's physician or advanced practice nurse."
That includes visits "for residents who are struggling with a change in environment, lack of physical family support, grief after a friend or family member passes away, weight loss or dehydration because the resident is no longer receiving cuing or encouragement to eat or drink from caregivers or family members, and emotional distress due to not talking or interacting with others."
The new rules also spell out quarantine requirements for workers and residents.
Workers required to quarantine can return to work after 10 days, or seven if they have a negative covid-19 test five days after the exposure.
Residents who are exposed to someone with the virus must quarantine for 10 days. A test for the virus at least seven days after the exposure is recommended, the rules say.
Residents who test positive should be isolated for 14 days, with that period extended to 21 days for those who have compromised immune systems or are in chemotherapy.
RIDING ON ELEVATORS
The Health Department on Wednesday afternoon also posted a directive on precautions that should be taken to avoid the spread of the virus on elevators and escalators.
Those include a requirement for people on elevators to wear masks. Signs should also be posted reminding people about the requirement.
"Ask elevator occupants to avoid speaking, when possible," the directive, dated Dec. 11, says.
It also says that people should be encouraged to take the stairs when possible, that floor markings should be used to indicate where people should stand while waiting to get on an elevator or escalator and that the number of people allowed on an elevator should be limited so that people can keep a safe distance from one another.
Signs should also tell people to avoid touching surfaces, the directive says. It says they should use an object, such as a pen cap, or their knuckle, to press the buttons.
OUTLOOK IMPROVES
While warning of a growing number of hospitalizations and deaths in coming months, projections released this week by the University of Arkansas for Medical Sciences' Fay W. Boozman College of Public Health showed an improved long-term outlook compared to the college's previous report two weeks earlier.
The latest forecast, dated Dec. 18, predicts active infections will peak at 27,868 on April 12 under a moderate scenario or 54,818 the same day under a worst-case scenario.
Those numbers include infections predicted to be confirmed through tests as well as those of people who don't get tested.
Of those with active infections during the peak under the moderate scenario, 1,839 were predicted to require hospitalization, including 643 who will need intensive care and 225 who will be on ventilators.
In a worst-case scenario, 3,617 were predicted to require hospitalization, with 1,265 in intensive care and 442 on ventilators.
The previous report, dated Dec. 4, predicted active infections would peak at 40,348 on March 24 under a moderate scenario or 70,037 on March 23 under a worst-case scenario.
The number predicted to require hospitalization ranged from 2,663 in the moderate scenario to 4,622 in the worst-case scenario.
"The lower confidence boundary remains extremely low, indicating a wide range of uncertainty in long-term projections," researchers wrote in the latest report.
"Because the COVID-19 vaccine is not expected to be widely distributed until at least April, we would not expect it to have a significant impact on the course of the pandemic until after that time," they added. "We should expect high active infection rates until the COVID-19 vaccines are widely distributed and administered."
The report also predicts the state's death toll from the virus will reach 3,751 by Feb. 15, which it says is an increase of 1,249 compared to the number at the end of November.
SCHOOL CASES
According to biweekly Health Department reports, the number of active cases among students and employees fell slightly from Monday to Wednesday at the state's public schools and higher education institutions while rising slightly at private elementary and secondary schools.
At public schools, the number of active cases fell by 117, to 2,904.
That drop came despite the cumulative number of cases rising by 666, to 24,049.
The increase included at least 386 new cases among students and 233 among employees. Those totals don't equal the overall total due to "unavailable data," according to the reports.
The number of school districts with at least five active cases fell from 151 as of Monday to 141 as of Wednesday.
The Springdale School District had the largest active-case total as of Wednesday, 123, followed by the Rogers School District, which had 102, and the Little Rock School District, which had 98.
At colleges and universities, the number of active cases among students and employees fell by 14, to 386, while the cumulative number rose by 112, to 9,912.
The University of Arkansas, Fayetteville had the most active cases as of Wednesday, 99, followed by the University of Central Arkansas in Conway, which had 35, and Arkansas Tech University in Russellville, which had 20.
Among private elementary and secondary schools, the number of active cases rose by 14, to 157, while the cumulative case total rose by 47, to 1,311.
Southwest Christian Academy in Little Rock had the most active cases among that group as of Wednesday, 31, followed by Shiloh Christian Schools in Springdale, which had 12, and Pulaski Academy in Little Rock, which had six.
'RED ZONE' DISTRICTS
Meanwhile, UAMS' Arkansas Center for Health Improvement this week listed 182 of the state's school districts as being in either the "red zone" or "purple zone" based on the number of new cases among residents within their boundaries.
That was up from 150 with one of the labels a week earlier.
The center, which describes itself as an independent health policy organization, listed 149 districts as being in the red zone, meaning that over a two-week span, they had 50-99 new cases per 10,000 residents who are not incarcerated or residents of nursing homes or state-run centers for the developmentally disabled.
An additional 33 districts were listed as being in the purple zone, meaning they had 100 or more new cases per 10,000 residents during the same period.
The Bay School District had the highest rate, with its 55 cases translating to a rate of 175 cases per 10,000 residents.
"What these numbers reflect is that Arkansas is experiencing uncontrolled spread of the coronavirus at a time when families, friends, and neighbors traditionally gather for holiday celebrations," the center's chief executive, Joe Thompson, said in news release.
"Our actions to break the spread of this virus are critical to our schools, hospitals, and communities."
Information for this article was contributed by Michael R. Wickline of the Arkansas Democrat-Gazette.