Although vaccination mandates stoked fears of labor shortages at U.S. hospitals, the health care systems that implemented them have touted widespread compliance.
Officials at some hospital systems that report high vaccination rates gave credit to the recent requirements. The officials said they have seen coronavirus infections -- and sick leaves -- noticeably drop.
[Video not showing up above? Click here to watch » arkansasonline.com/1017desantis/]
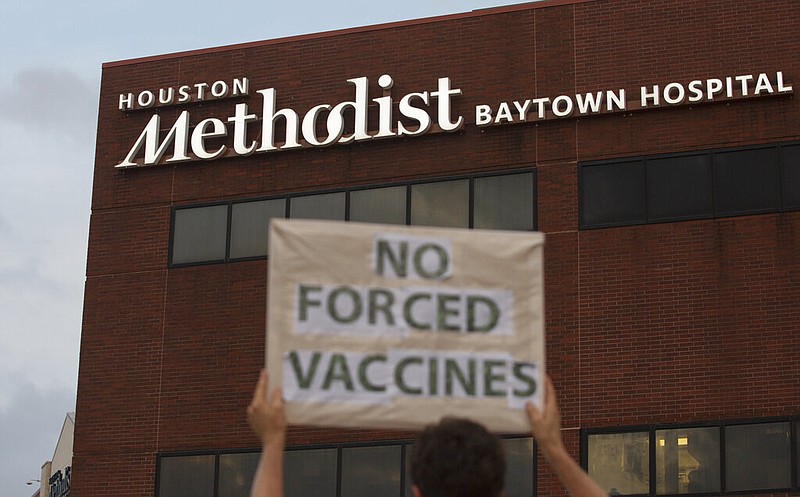
Houston Methodist, one of the first American health care institutions to require workers to get vaccinated against the coronavirus, faced backlash against its mandate.
More than 150 employees were fired. There were legal battles and protests.
But President and CEO Marc Boom said he has no regrets because 98% of current staff members have been vaccinated, and they and the patients are safer as a result.
"I can unequivocally say [it was] the best decision we ever made," Boom said in an interview.
About 41% of hospitals nationwide -- roughly 2,570 facilities -- have some sort of vaccination mandate, according to data collected by the American Hospital Association. Others are expected to follow after President Joe Biden announced last month that he would require most health care facilities that accept Medicaid or Medicare funding -- many of which also treat immunocompromised people who are at high risk of getting severely ill from covid-19 -- to vaccinate their employees.
At Novant Health, a 35,000-employee health care system in four Southeast states, more than 99% of workers have complied with a vaccination mandate, spokeswoman Caryn Klebba wrote in an email.
"Without a vaccine mandate for team members, we faced the strong possibility of having a third of our staff unable to work due to contracting, or exposure to, covid-19," she said. "This possibility only increases heading into a fall season with the more contagious and deadly Delta variant."
[Video not showing up above? Click here to watch » arkansasonline.com/1017antibodies/]
But many hospitals still lack mandates, and efforts to vaccinate every eligible staff member have lagged. Some officials worry that staff members, overwhelmed from the summer delta variant surge, could remain exposed as the U.S. faces a potential "twindemic" of covid-19 and flu spikes this winter.
The federal government does not require health care facilities to share their vaccination data. But at more than 2,000 facilities nationwide that voluntarily reported numbers to the Department of Health and Human Services, approximately 25% of hospital workers were unvaccinated, according to data provided last month.
Even at some hospitals that have not yet mandated shots, administrators have touted their vaccination rates.
But the unvaccinated minority of hospital workers have drawn the public's attention with their vocal opposition in the form of protests and lawsuits. Hospital workers have filed or joined lawsuits in at least eight states -- including Oregon, Minnesota and New York -- against employers or public agencies over vaccination mandates.
Houston Methodist made headlines over the summer for suspending 178 employees who did not get vaccinated -- after a judge dismissed a lawsuit from 117 employees who challenged the mandate, alleging it was reminiscent of Nazi-era "nonconsensual human experimentation."
Boom said the headlines belie the fact that less than 0.6% of Houston Methodist's 26,578 employees quit or were fired because they refused to get vaccinated.
Texas Gov. Greg Abbott, a Republican, issued an executive order Monday to ban any entity in the state, including private businesses, from requiring vaccinations for employees or customers. Boom said he was "grateful" that the hospital had mandated vaccinations early, "so the order will not have an immediate impact."
Jared R. Woodfill, a lawyer representing workers who were terminated, said in an interview and in a letter sent to the hospital that Abbott's order applies to his clients and that they should be reinstated -- an argument that he said he plans to make in his ongoing lawsuits against the hospital in state and federal court.
Stefanie Asin, a hospital spokeswoman, said, "There is no merit to what he is saying."
The hospital will not rehire the unvaccinated former employees, Asin said.
Boom credited the widespread vaccinations with keeping 300 workers from getting sick over the summer, according to an analysis the hospital conducted of short-term disability leaves.
Staff members who did get sick with covid-19 reported less severe cases, Boom said, and no employees died over the summer. Houston Methodist lost two workers to covid-19 in summer 2020.
Despite the clinical and real-world evidence that vaccination not only protects the people who get their shots but also those around them, some hospital workers have still declined to get vaccinated, leaving hospitals in some parts of the country struggling to persuade them.
Arnhild Espino, a registered nurse at Legacy Mount Hood Medical Center in Gresham, Ore., was put on unpaid administrative leave Sept. 30 for refusing to get vaccinated. She was among 794 of 14,000 workers who were not yet vaccinated. Espino is searching for employment elsewhere and is considering seeking a license in Florida, where vaccination requirements are less strict.
After Abbott's order, Florida Gov. Ron DeSantis, a Republican, pledged in a news conference to explore options to prevent employers from firing workers for not getting vaccinated.
"Oregon state is stripping away my livelihood and everything I hold true," Espino said.
Since Espino and others were put on administrative leave, 114 employees have come into compliance and 97 are on their way to becoming fully vaccinated, Legacy spokeswoman Kristin Whitney said. Still, the system of six hospitals and about 70 clinics has temporarily consolidated or closed services, including CT, mammography and ultrasound, at about 10 facilities to lessen the burden on staff members while employees are on leave.
There were 986 exemption requests, of which at least 897 were denied, according to an internal presentation shared with The Washington Post.
One nurse in Washington state, who spoke on the condition of anonymity because her employer does not allow employees to speak to the media, had initially sought an exemption and was denied and suspended.
The nurse said she considered going into child care. Her family sold one of their cars, and she weighed applying for food stamps. Unemployment was not available to those who lost their jobs because they declined to get vaccinated, she said.
But after taking a break from social media, praying and talking to her husband about the financial risks of losing her well-paid job, she said, she changed her mind. Now she plans to get vaccinated and return to work.
Workers leaving their jobs are also reckoning with stepping away from hospitals at a time when staffing is most needed.
LOSING WORKERS
When asked what a loss of 1% of health care workers could look like in New Mexico, which has mandated vaccination for those employees, David Scrase, the acting head of the state's Health Department, said the impact on an already strained system is considerable. But he added that even if unvaccinated workers kept their jobs, they could be out for long periods if they became infected and got seriously ill.
"A 1% impact on health care workers in our state would mean that all the other health care workers would have to work 1 harder," he told reporters on a call last month. "They're already working as hard as they can, so I think it's a big deal."
Gov. Tim Walz of Minnesota said Friday that he would call upon the state's National Guard to help ease staffing shortages that have kept hospitals from transferring covid-19 patients for stepped-down care at long-term care facilities.
Walz called the transfers a "very typical thing in our medical system" and said they had been bottlenecked by capacity at those facilities. He said the National Guard will be given the training necessary to provide long-term care. He did not say how many soldiers will provide that relief but noted that it will be "a fairly large contingent."
Dr. Kevin Croston, CEO of North Memorial Health Hospital in Robbinsdale, Minn., said his organization was struggling with staff shortages it did not have a year ago. "Our teams are now more stressed than they've ever been," he said, adding that the "roller coaster" his employees are experiencing is happening all over Minnesota.
Earlier this month, the state's health commissioner, Jan Malcolm, said the staffing shortages among health care workers stemmed from "the extreme stress and burnout that they have faced for over 18 months now."
The state is facing another surge of cases. The number of hospitalized patients infected with the coronavirus is nearing 1,000, according to state data. Cases in Minnesota are up 20% in the past two weeks, as are hospitalizations, according to a New York Times database.
Walz said 400 of the patients hospitalized for covid-19 should be transferred to lower-level care, but beds at those facilities are not available -- and those 400 hospital patients are taking up space needed for incoming patients.
The state also announced that an emergency staffing pool would be reactivated, a measure used earlier in the pandemic.
State Rep. Anne Neu Brindley, a Republican, issued a statement Friday saying Walz's plan was "merely a Band-Aid that won't outweigh destructive government policies," according to the Minneapolis Star Tribune. She said policies such as vaccination mandates are "driving health care worker resignations and layoffs."
The high compliance numbers that many hospitals cite do not always tell the full story. Some hospitals are more lenient than others in granting exemptions, which may lead to a larger share of unvaccinated staff members choosing to skip vaccination without losing their jobs.
GRANTING EXEMPTIONS
About 10% of the 20,000 employees of MUSC Health, the clinical network of the Medical University of South Carolina, received permission to skip vaccination for religious or medical reasons, according to Patrick Cawley, its CEO. In a typical flu season, less than 1% of MUSC Health employees are exempt from the influenza vaccine, Cawley said.
Unlike some other hospitals that set up committees to examine exemption requests for merit and decide whether to grant them, MUSC Health "did not do that," Cawley said.
Other hospital networks have reported small fractions of workers receiving exemptions. Less than 4% of UNC Health's 30,800-person workforce was granted religious or medical exemptions, according to Matthew Ewend, the chief clinical officer of the state-owned network of 14 hospitals, 18 hospital campuses and more than 500 clinics in North Carolina.
Ninety-nine percent of the workforce is vaccinated or exempt, Ewend said, but the system could lose nearly 300 staff members if they don't get vaccinated by Nov. 2, the end of a probationary period.
"We're talking a lot about the 2% who aren't in compliance, but a huge swath of our workforce came into compliance, and not only did that, but did it willingly," Ewend said. "And I think their voice sometimes is lost because we are thinking about the folks who have struggled with this."
Information for this article was contributed by Meryl Kornfield and Annabelle Timsit of The Washington Post and by Lauren McCarthy of The New York Times.