Drafting volunteer and paid medics and scribes will help Arkansas hospitals treat more patients, health officials say.
Arkansas needs to expand its hospital capacity to meet the anticipated needs of covid-19 patients, officials have said. That means more beds and more people.
Gov. Asa Hutchinson said last week that state officials expect 3,500 people to be infected in two weeks, with 700 of them -- 20% -- needing hospitalization. On Tuesday, he said the state's current trajectory means it might fall short of that projection. Still, the state continues to work with the National Guard and the U.S. Army Corps of Engineers on finding new places to house patients.
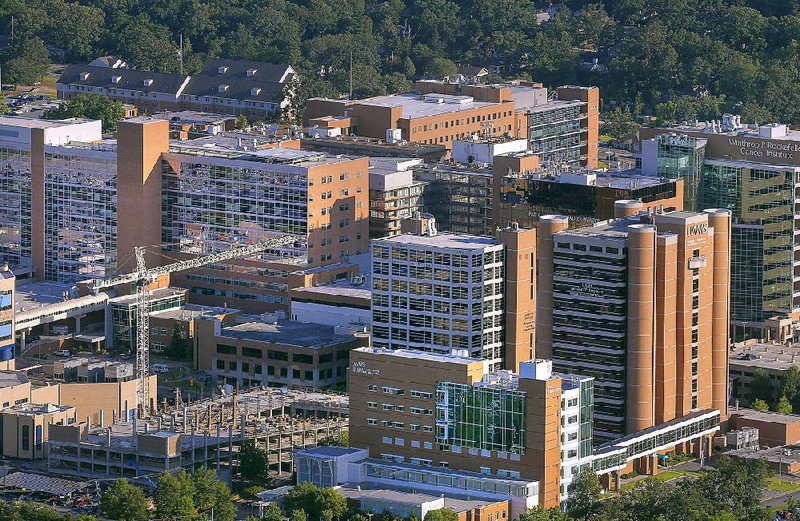
The University of Arkansas for Medical Sciences has several plans in place, Chancellor Cam Patterson said, if it happens that more people go to the hospital than it can handle.
"I think it almost certainly will," Patterson said.
His ideas are similar to those at the state level and at Baptist Health, according to interviews.
[60% of people are infected in 6 months] [40% of people are infected in 6 months] [20% of people are infected over 18 months]
ARKANSAS: Percentage of available beds needed if
[60% of people are infected in 6 months] [40% of people are infected in 6 months] [20% of people are infected over 18 months]
[Maps not loading above? Click here to see them: arkansasonline.com/41beds]
Some of those ideas include bringing in outside people as extra staff members; reallocating bed space no longer used by people having elective procedures; repurposing staff members from those areas to covid-19 cases; hiring people to be scribes so doctors and nurses don't have to do so much paperwork and can see more patients; and, across Arkansas, looking for other hospitals or new spaces to house patients, such as closed hospitals.
Hospital staffing will be a priority, Patterson said. About 100 UAMS staff members are quarantined because of covid-19, chiefly because they've been directly exposed.
Problems could get worse soon at Baptist Health, where President and CEO Troy Wells has announced layoffs and reduced hours. The hospital is earning less money from patients and their insurance while they postpone elective procedures to prevent infections.
But Nate Smith, secretary of the state Department of Health, remained optimistic that eventually hospitals will be fine.
"In some sense there will be an influx of money if hospitals are getting paid and seeing more patients," he said.
In an email Tuesday, UAMS spokeswoman Leslie Taylor called the reduced services while awaiting covid-19 patients "a delicate balance."
To help curb exposure within the hospital and to keep medical staff and work, UAMS has purchased a $350,000 "super fan" that will make the hospital's ninth floor a "negative pressure" unit, meaning the air circulated there will stay there.
That's where officials plan to house covid-19 patients. That floor has 60 beds. An existing negative-pressure unit of 42 rooms on a different floor is dedicated to treating covid-19 patients. All rooms can be double-occupancy, if needed.
Canceling elective surgeries has freed up beds already, but some models project even that won't keep the state from having more patients than bed space based on current conditions.
But Smith said existing models projecting infection rates or beds needed don't account well for geographic differences among states or regions.
Places like New York City, where the outbreak is the worst so far, are more densely populated, making it harder for people to distance from one another. People rely on public transit and walking. In contrast, Arkansas is one of the most rural states in the nation, and it has far fewer people who rely on public transit in its more urban areas.
The models are also making longer-term projections based on shorter-term data, Smith noted.
"We really don't have much experience with this virus," he said.
So, Smith said, the projections for Arkansas, while still alarming, may be worse than what will actually happen.
"People are going to be hearing different numbers with respect to case burden," Patterson said. "This is going to get substantially worse before it gets better. The issue that's difficult to predict is how difficult is it to apply data that's primarily drawn from large metropolitan areas and apply it to less dense places."
Various entities, including UAMS, are working on a model that will better reflect Arkansas' reality.
Data from the Harvard Global Health Institute and the Harvard T.H. Chan School of Public Health projects anywhere from 51% of available hospital beds being needed to 469%. The low end is if 20% of the state's population is infected in an 18-month time span, and the high end is if 60% is infected in a six-month time span.
Researchers made nine projections, based on 20%, 40% or 60% of residents infected over six-month, 12-month or 18-month time periods.
If hospitals can cut their numbers of non-coronavirus patients in half, those projections range from 33% to 305%.
The likelier scenario, Smith said, is the one in which 40% of the state's residents are infected within six months. But he doubts the percentage will be as high as 40%. In that scenario, three times as many beds will be needed than are available. It's reduced to twice as many if hospitals cut their numbers of non-coronavirus patients by half.
"Forty percent may be high, but I'd rather us shoot for that," Smith said.
Additional staffing can come from people not scheduled to work or from community members who have signed up to be used in emergency cases. People who can take notes for nurses or doctors can free up those nurses and doctors to see more patients.
Typically, the burden of paperwork is much higher in the United States, and doctors can't see as many patients, Smith said.
Wells, the president and CEO of Baptist Health, said other people in the community with medical expertise could be consulted using varying technologies. He gave an example that a retired pulmonologist, who would be at risk for covid-19 complications, could consult doctors or patients at the hospital remotely.
Some people who could help may be those with nursing or EMT licenses who aren't actively using them, Smith said.
Other ways to allow for more beds include doubling up rooms, Smith said. Instead of one person to a room, patients could be housed together.
[CORONAVIRUS: Click here for our complete coverage » arkansasonline.com/coronavirus]
He recalled his time working in Kenya years ago. There, medical workers might be treating 40 people in a space "that in the U.S. you might put five people in."
Still, he said, it's not ideal.
"But if everyone has the same illness, you're not really concerned about" disease transmission, he said.
Metro on 04/01/2020