After increasing by double digits this year, the rates for plans sold on Arkansas' health insurance exchange would increase an average of less than 5 percent next year under requests submitted by the insurance companies, the state Insurance Department announced Friday.
Arkansas Blue Cross and Blue Shield requested an average increase of 4.4 percent for its plans covering 186,510 people, according to the department.
St. Louis-based Centene Corp., which sells plans under the name Ambetter Arkansas and has plans covering 85,373 people, requested an increase of 4.6 percent.
Little Rock-based QualChoice Health Insurance requested an increase of 1.5 percent for a group of plans covering 16,013 people and 1.06 percent for another set of plans covering 14,996 people.
Insurance Commissioner Allen Kerr will rule on the requests by Aug. 23. If approved, the increases would take effect Jan. 1.
"This round of initial requests places Arkansas among the lowest in the country and shows that the health insurance market in Arkansas remains stable," Kerr said in a news release.
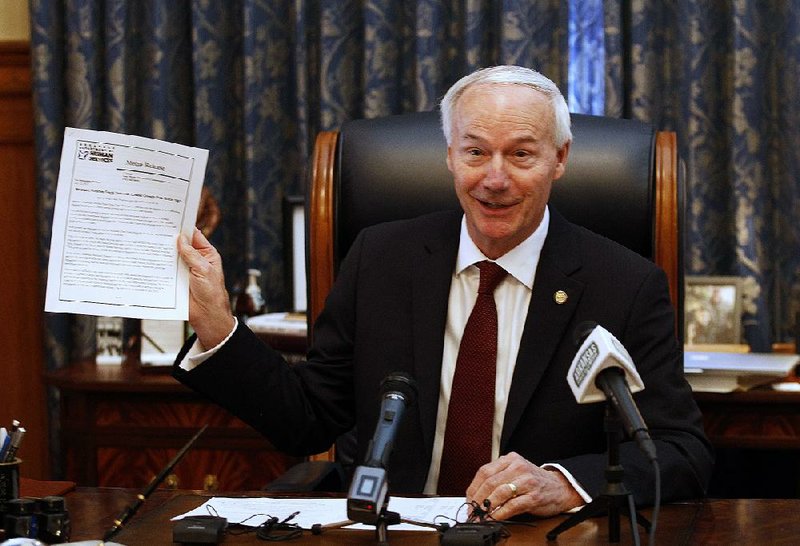
Gov. Asa Hutchinson mentioned the rate requests during an afternoon news conference Friday touting achievements of his administration.
"For those who have followed this in previous years, that is a significant reduction in the annual increase that is being requested," he said.
Created under the 2010 Patient Protection and Affordable Care Act, the insurance exchange offers plans to consumers who buy coverage on their own rather than through employers, and allows them to apply for subsidies to help pay for it.
Under the so-called private option, Arkansas also buys coverage in such plans for people who became eligible for Medicaid under that program's expansion in 2014.
The federal waiver authorizing Arkansas Works, as the expanded part of the Medicaid program is known, limits the private option's cost based on a monthly, per-enrollee cap. That cap is set to rise 4.7 percent next year -- just more than the increases requested by the two insurance companies with the largest numbers of customers.
State officials don't yet know what effect the increases would have on the private option's cost, said Marci Manley, a spokesman for the Department of Human Services, which oversees the Medicaid program.
Joe Thompson, director of the Arkansas Center for Health Improvement, noted that the higher increases this year came in response to President Donald Trump's decision to eliminate a federal subsidy for insurance companies.
Typically, he said, rate increases in Arkansas have been lower than in other states because of the private option, which guarantees insurance companies a large pool of customers.
In June, about 237,000 of the people covered by exchange plans were enrolled through the private option.
"If we don't have another major destabilizing event, the Arkansas insurance market looks very good compared to others across the nation," Thompson said.
This year, the rates increased an average of 14.2 percent for Blue Cross plans, 21 percent for Centene plans and about 25 percent for QualChoice plans.
The subsidy eliminated by Trump reimbursed insurance companies for providing enhanced coverage to low-income consumers enrolled in so-called silver-level plans.
Silver plans normally cover about 70 percent of a typical consumer's medical expenses, but they cover a higher percentage for consumers with incomes of less than 250 percent of the poverty level, or less than $42,490 for an individual or $87,850 for a family of four.
Insurance companies increased the premiums for the silver-level plans to offset the loss of the subsidy, known as cost sharing reduction payments.
"The most important assumption continues to be that we are assuming that the federal [cost sharing reduction payments] will continue to not be paid; therefore, the expense must be borne by insureds utilizing Silver benefits," Arkansas Blue Cross and Blue Shield said in an Insurance Department filing.
Last year, the company collected more than $1 billion in premiums for its plans sold on the individual insurance market, including exchange plans, and paid $793.7 million in claims, according to another filing.
Next year, it said, it expects to collect $701.7 million in premiums and pay out $584.9 million in claims.
"The overall trend is around 6.6%; however, the claims experience is coming in better than anticipated in 2018, leading us to believe that the cost for 2019 will not increase at the same level," the company said in a filing.
A Section on 08/04/2018