The state Legislature on Wednesday gave final approval to bills endorsing a plan to remove about 60,000 Arkansans from the state's expanded Medicaid program and impose a work requirement on many of those who remain enrolled.
The identical bills, House Bill 1003 and Senate Bill 3, were sent to Gov. Asa Hutchinson on the third and final day of a special legislative session focused mostly on health care matters.
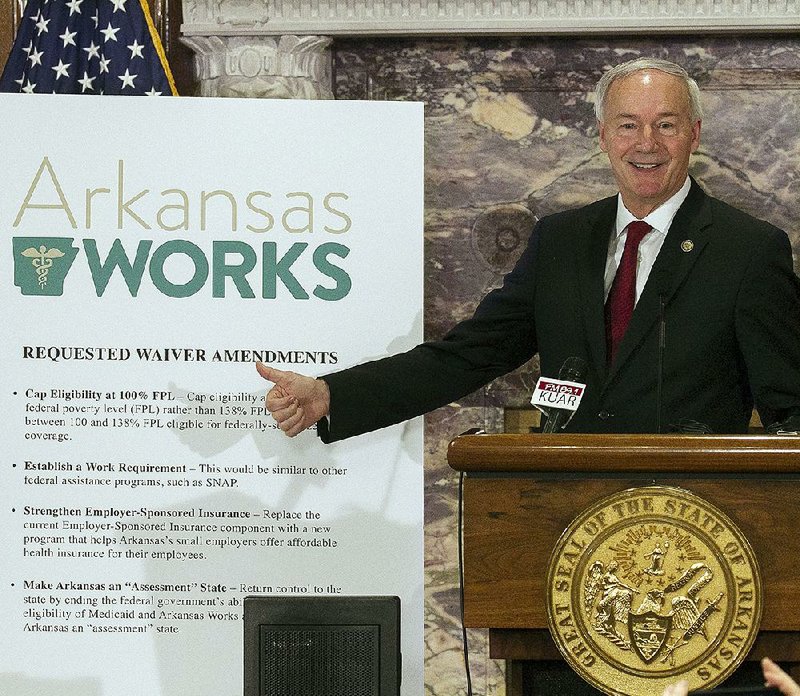
Hutchinson said he likely would sign the bills today.
The legislation is designed to save the state money by limiting eligibility for the expanded part of the state's Medicaid program, known as Arkansas Works, to adults with incomes of up to 100 percent of the poverty level, instead of the current threshold, 138 percent of the poverty level.
State officials have said that would result in the removal of about 60,000 of the 320,000 Arkansans covered by the program to provide health care coverage.
If the changes cause more low-income Arkansans to go without insurance, hospitals could be forced to provide millions of dollars more in unreimbursed care, according to state Department of Human Services projections.
For instance, if half the 60,000 Arkansas Works enrollees end up going without health insurance, the cost to hospitals of providing them unreimbursed medical care would be $28 million next year, when the department plans to phase in the eligibility change at a rate of about 5,000 enrollees per month, according to the projections.
In 2019, when the eligibility change is fully implemented, the cost would be about $53 million, the department said.
On the other hand, if only 10 percent go without coverage, the cost to hospitals would be $5.6 million next year and $10.6 million in 2019, according to the projections.
The department provided the figures to the Arkansas Democrat-Gazette on Wednesday in response to a request under the Arkansas Freedom of Information Act.
Hutchinson said the state will work with insurance companies and health care providers to ensure a "smooth transition to move those that are moving off of Arkansas Works" into federally subsidized coverage in non-Medicaid plans.
"We want to make sure that any impact on our rural hospitals for uncompensated care is negligible," Hutchinson said. "I'm confident that we're going to do everything that we can to make sure that that happens."
With Republicans in the U.S. House of Representatives continuing to work on legislation that would repeal much of the 2010 Patient Protection and Affordable Care Act, including cutting off enhanced funding to states, such as Arkansas, that expanded Medicaid, Hutchinson said he was "more confident than ever that we're doing the right thing by moving forward with our reform now."
"We're in a position to make adjustments now that I believe will fit in very well with the reform efforts that they're trying in Washington," Hutchinson said. "I think that we will be a national leader in this effort."
Department officials have said they will submit an application to President Donald Trump's administration in the next month for a waiver allowing the changes, which, if approved, would take effect as early as Jan. 1.
According to a department timeline distributed to lawmakers, a draft of the waiver application will be released this month, and rules implementing the changes will be submitted to the Legislative Council in August. The council meets when the Legislature is not in session, and it oversees executive branch actions.
The House approved SB3 69-21 after passing HB1003 in a 71-23 vote a day earlier. The Senate, which approved SB3 in a 23-9 vote on Tuesday, approved HB1003 19-7.
Nearly all the bills' support came from Republicans, with opponents including most Democrats and a few Republican opponents of Medicaid expansion.
SB3 did get the support of one Democratic House member: Rep. Eddie Armstrong of North Little Rock, who didn't vote Tuesday on HB1003.
In the Senate, Democrat Eddie Cheatham of Crossett supported the legislation in votes Tuesday and Wednesday. Democratic Sen. Stephanie Flowers of Pine Bluff voted in favor of the Senate version but didn't vote Wednesday on its House counterpart.
Under the so-called private option, most Arkansas Works enrollees are covered by private plans offered on the state's health insurance exchange, with Medicaid funds paying most or all of the premium and providing additional subsidies that reduce the recipients' out-of-pocket spending for medical care.
Most or all of the 60,000 Arkansans Works enrollees with incomes of 100 percent to 138 percent of the poverty level would become eligible for federal tax credits to help pay for coverage under the same plans, or other exchange plans of their choosing, once they become ineligible for Medicaid.
The assistance provided by the tax credits varies according to a consumer's age, family size and income, and the price of available plans, and it likely would be less generous than the Medicaid subsidies.
For instance, if Arkansas had not expanded Medicaid, a single, 40-year-old Pulaski County resident with an income of 100 percent to 138 percent of the poverty level would have qualified for a monthly tax credit this year ranging from about $264 to $272.
The premium for the cheapest "silver"-level plan -- offering coverage comparable to Arkansas Works plans -- that would be available to that consumer has a premium of $292 a month, meaning the consumer's premium would range from $20 to $28 after the tax credit is applied.
Under Arkansas Works, all of the 60,000 enrollees who are in private-option plans are charged premiums of $13 a month.
The tax credit for the 40-year-old consumer would cover the entire premium for a cheaper, "bronze"-level plan, but the deductible would be at least $5,000.
The more expensive plan, like private-option plans, would have no deductible because of additional federal subsidies that kick in for silver-level plans.
Paying premiums is also more important for enrollees in non-Medicaid plans. Those who fail to pay for 90 days will lose their coverage and will be unable to enroll again until the next annual open-enrollment period.
Arkansas Works enrollees who fail to pay their premiums accrue a debt to the state but don't lose coverage. Department of Human Services Director Cindy Gillespie said last week that about 75 percent of private-option enrollees are behind on their premiums.
Marquita Little, health policy director for Arkansas Advocates for Children and Families, said in an interview Wednesday that there's a "high probability" that a similar percentage of Arkansas Works enrollees who lose Medicaid eligibility will end up going uninsured.
She suggested the state automatically enroll those people in the non-Medicaid plans.
The state should also refer the enrollees to community organizations that can answer questions about enrollment and choosing a plan, and it should cover the difference in the premiums and cost sharing for the non-Medicaid plans during a six-month transition period, Little said.
Human Services Department spokesman Brandi Hinkle said providing Medicaid subsidies during such a transition period is not "part of the waiver that we've been asked to submit," but that the department will consider such recommendations as it crafts its waiver request and implementation plan.
Before the expansion took effect in 2013, Medicaid eligibility in Arkansas was restricted mostly to children from low-income families, parents with incomes of up to 17 percent of the poverty level and poor people who are elderly or disabled.
Under the Affordable Care Act, the federal government paid the full cost of coverage through 2016 for the newly eligible adults in states that expanded Medicaid, but the states became responsible for 5 percent of the cost this year. The states' share is scheduled to rise every year until it reaches 10 percent in 2020.
Restricting Medicaid eligibility to those at or below the poverty level would save the state between $66 million and $93 million from fiscal 2018, which starts July 1, through fiscal 2021, the Human Services Department estimated.
The Legislature on Wednesday also gave final approval to bills that would abolish the Arkansas Health Insurance Marketplace Legislative Oversight Committee and shift that committee's duties to the Legislative Council.
Created by the Legislature in 2013, the marketplace established a state-run health insurance exchange for small businesses and approves plans offered in the health insurance exchange for individual consumers.
House Bill 1004 and Senate Bill 4 also would direct the council to conduct a study of the marketplace's future.
Information for this article was contributed by Brian Fanney of the Arkansas Democrat-Gazette.
A Section on 05/04/2017